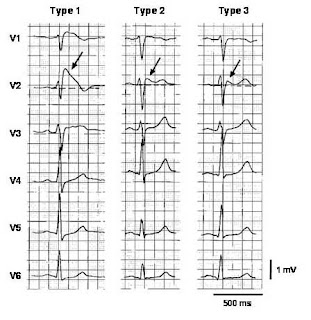
OK, Right bundle branch block ( RBBB) is certainly a favourite ECG finding your consultant would like to show you during grand round.
This blog is written for those who are preparing for MRCP Part 1 and2! Free MRCP Resource Blog!
Wednesday, January 19, 2011
RBBB in MRCP
OK, Right bundle branch block ( RBBB) is certainly a favourite ECG finding your consultant would like to show you during grand round.
Wednesday, January 12, 2011
Whipple's Disease in MRCP
Yes, you are right, Whipple's disease is rare but not in your MRCP Part 1 and 2 examination. I myself never diagnosed Whipple's disease before but this illness is ceratinly a all time favourite in MRCP examination.
 Although Whipple's disease primary leads to GIT syndrome ( diarrhoe,weight loss) but for MRCP, patients with Whipple's disease is usually illustrated with symptoms of joint pain!
Although Whipple's disease primary leads to GIT syndrome ( diarrhoe,weight loss) but for MRCP, patients with Whipple's disease is usually illustrated with symptoms of joint pain!Sunday, January 09, 2011
Iron Deficiency Anemia
In my last post, I talk about iron metabolism in MRCP, as you all know, iron is an important ingredient in heme synthesis. Therefore iron deficiency leads to anemia ( hypochromic,microcystic anemia) which is a type of anemia manifested by small red cells ( low MCV- mean corpuscular volume) and pale red blood cells ( low MCHC- mean cospuscular hemoglobin concentration).
Iron deficiency is diagnosed by diagnostic tests as a low serum ferritin, a low serum iron level, an elevated serum transferin and a high total iron binding capacity (TIBC).
So what causes iron deficiency anemia- yes, it is mainly due to chronic blood loss and the main cause worldwide is worms infestations! (hookworms, whipworms, roundworms). However, another reason for chronic blood loss is GIT bleeding, therefore, for anyone older than 50 years, always think of the possibility of GIT malignancy!
One thing to take note, Thalassemia minor also has the similar lab results as iron deficiency and you must always consider Thalassemia as your differential diagnosis in iron deficiency anemia!
Tuesday, January 04, 2011
Iron Metabolism for MRCP
 There are a few important fact to remember for MRCP,
There are a few important fact to remember for MRCP,
Friday, December 31, 2010
Happy New Year!!

Friday, December 17, 2010
Liddle's syndrome in MRCP
I must say that there are a few genetic renal transport disorders which are popular in MRCP part 1 and 2. These are Bartter's syndrome, Gitelman's syndrome and of course Liddle's syndrome.
Liddle's syndrome is one of the rare causes of secondary hypertension. For you to understand better, you must know that our body maintains fluid balance mainly by controlling sodium homeostasis. However about 25000 mmol of sodium is being filtrated from our kidney everyday and it is crucial that majority of the sodium is being reabsorped from the tubule.
Although collecting duct is only responsible for 1-2% of total sodium reabsorption, it is the major site for our body to control the fluid status because it is the only site that is sensitive to our body hormone ( aldosterone)

Sodium is mainly being reabsorped via Sodium channel ( ENAc) at collecting duct. When aldosterone binds to mineralcorticoid ( MR) receptor, more ENac will be synthesized and more sodium will be reabsorped and more pottasium being excreted ( that explaines why primary aldosteronism patients have hypertension and hypokalemia)
Liddle's syndrome is just a genetic disorder when the ENac is activated all the time and sodium reabsorption is enhanced leading to hypertension and hypokalemia.
Hypokalemia and Hypertension
We are always reminded that when a patient is diagnosed to have hypertension, the possibility of secondary hypertension must be entertained especially for young patients.
There are various clues that can lead us to suspect a patient might have secondary causes and one of them is hypokalemia.
Therefore, if you find a patient with hypertension and hypokalemia, always think of the following diagnosis,
1) Renal Artery stenosis or renin secreting tumor ( RAS)
2) Liddle's syndrome
3) Adrenal hyperfunction- can be due to adrenal ademona/carcinoma leading to hyperaldosteronism
4) Licorice usage or syndrome of apparent mineralcorticoid access ( SAME)
And one of the popular question in MRCP is how to differentiate these four conditions!!
It is quite easy if we know how renin angiotensin aldosterone ( RAA) system works. It is summarised as the following image,
 For RAS or renin secreting tumour, you will have high renin and high aldosterone. For aldrenal hyperfunction, patients have high aldosterone level but normal renin.
For RAS or renin secreting tumour, you will have high renin and high aldosterone. For aldrenal hyperfunction, patients have high aldosterone level but normal renin.
As for Liddle's syndrome and SAME, I will try to explain a bit deeper next time!
Tuesday, November 16, 2010
Pancytopenia for MRCP
Recently I saw a patient with pancytopenia in my ward. A 24-year old ESRF gentleman on CAPD for the past 4 years ( with primary disease of SLE) came to us with fever and joint pain. Full blood count showed a Hb of 4.5, TWC of 1.2 and Plt count of 45.

As we all know, bone marrow produces red cell, white cell and platelet. Pancytopenia just means a condition with reduction of all these three cell types.
It is always interesting to find the underlying cause for pancytopenia and I always try to remember the causes as the following order,
1) Inability for production/Infiltration of bone marrow
- Certainly one of the commonest cause is leukaemia, however, you have to always bear in mind the possibility of aplastic anemia. In older patients, always consider the possibility of bone marrow infiltration by tumour due to secondaries. Severe folic and Vitamin B12 also can cause pancytopenia but frankly speaking, I have never encountered one in my life!
2) Consumption
- although the production in the bone marrow is normal, all these cells can be broken down ( consumed) in the periphery. This can happen either in the spleen ( due to hypersplenism) or in circulation because of autoimmune respond ( due to underlying autoiimune disease)
3) Drugs
- certain drugs or even some infections can cause bone marrow suppression leading to pancytopenia. Popular drugs include choramphenicol, azathioprine ( especially used with allupurinol). Various infections can lead to pancytopenia but always remember about Parvovirus b 19.
Back to our patient, he actually has azathioprine induced pancytopenia. However, pancytopenia due to SLE should be entertained as well!
The worrying thing about pancytopenia is of course managing the neutropenic sepsis if it occurs. My patient actually developed neutropenic sepsis and he was treated with broad spectrum antibiotics. His cell counts improved after azathioprine was stopped.
Monday, October 25, 2010
Hemoglobinuria or myoglobinuria
I always confused these two conditions when I was a medical student. Now let me make these conditions as simple as possible.

Hemoglobinuria just means presence of hem in the urine whereas myoglobinuria means presence of myoglobin in the urine. Both can cause acute kidney injury due to pigment nephropathy.
Remember that both can cause a false positive in urine dipstick for RBC. Patients with both these conditions produce tea coloured urine. However myoglobinuria may be differentiated from hemoglobinuria by performing a series of simple tests.
-Myoglobinuria is brown, and often only a few RBCs are present in the urine.
-Hematuria produces a reddish sediment in spun urine samples.
-Red or brown urine with a negative dipstick result for blood indicates a dye in the urine.
-Hemoglobin produces a reddish or brown coloration in the spun serum, whereas myoglobin does not discolor the serum.
-CK levels are markedly elevated in myoglobinuria.
be jaundiced. These features have developed since he developed a mild chest infection one week ago. Which one
of the following is the most likely haematological finding?
2 ) low mean cell volume
3 ) Positive direct antiglobulin test
4 ) Reduced reticulocyte count
5 ) Spherocytes present on blood film
Wednesday, October 20, 2010
Vasculitides in MRCP
Let me makes this topic a very simple one, you just to know two conditions in this topic- Wegener Granulomatosis and Chrug- Strauss Disease.
Anyway, before we zoom in into these two conditions, I think candidates need to know this topic as a whole, vasculitis just means inflammation of blood vessels with reactive damage to the wall which can lead to downstream ischemia and necrosis.
Classification of vasculitis is depending on the size of vessel involved. You might want to know more about Chapel Hill Classification- either big vessel, medium or small vessel.
However, I do not think you need to know all these conditions- for MRCP candidates- big vessels vasculitis, you need to know Giant cell arteritis, medium size vasculitis- you need to know polyarteritis nodosa and small vessel disease- of course you MUST know Wegener Granulomatosis (WG) and Churg-Strauss Disease ( CS)
I will talk about Giant cell arteritis and polyarteritis nodosa next time and for today, we will put emphasis on WG and CS.

Since both involve small vessels, multiple organs can be involved, however, just remember the following similarities and differences between these two conditions.
Both of WG and CS can cause pauci immune glomerulonephritis and the classical finding is cresentric GN on biopsy
Both can be ANCA positive but WG is mainly c-ANCA and CS is mainly p-ANCA
WG patients usually have upper respiratory airway problem and can be misdiagnosed as nasopharygeal carcinoma or tuberculosis.
For CS, patients might present with asthma and usually has eosinophilia.
Yes, you are right, that’s all you need to know!!
Monday, October 18, 2010
Tumour Lysis Syndrome in MRCP
OK, this is a popular problem you see during your internship if you are working in an oncology ward. Remember that it is a MEDICAL EMERGENCY!
Tumor lysis syndrome (TLS) describes a condition with significant clinical and lab abnormalities caused by rapid and massive tumor cell death. Occurring either spontaneously or after chemotherapy. Therefore, it is quite logical to get this in patients with very high tumour load ( such as leukemia or lyphoma with very high white cell load)
You always encounter this syndrome post chemotherapy and always suspect this if patient develops acute kidney injury and hyperkalemia post chemotherapy.
Due to massive cell lysis, you will anticipate patients to have hyperkalemia, high phosphate and high uric acid with low Calcium.
Sometimes, patients might just present with seizure or cardiac arrthymias.
The pathogenesis of acute kidney injury is not so important for MRCP Part 1 and 2. Anyway you might get some ideas from the photo below,

About the amanegement, it is easy, the principles are below,
1) Adequately hydrate patient to prevent cystals formation
2) Prevent/minimize uric acid formation by giving allupurinol or rasburicase.
and of course sometime, you might need to dialyse the patient.
Sunday, April 18, 2010
MRCP Mock Exam (2)
More questions......
Question 1:
A 45-year-old man presented with diplopia, dysarthria and difficulty with swallowing. Over the next few days he developed weakness of the upper and lower limbs. On day 4 he was unable to walk unaided. He denied any sensory symptoms or bladder disturbances. His previous medical history is unremarkable. He is a non-smoker, does not drink alcohol excessively. He does not take any drugs .
On examination he was apyrexial. His general medical examination was normal. His higher mental function was unremarkable. There were no signs of meningism. Cranial nerve examination showed bilateral dilated and fixed pupils. He had binocular diplopia but
no obvious ophthalmoplegia. He was dysarthric with weak cough. His vital capacity was 3.15 standing and 2.00 lying flat. He had lower motor neuron tetraparesis of power 3/5. He was hyporeflexic with normal sensation. He was unable to walk unaided.
Blood tests including FBC, U+Es, LFTs, TFTs, Ca, Autoantibody screen, ESR,
CRP were normal. ECG and CXR were unremarkable. CT brain was normal. Nerve conduction studies and EMG were normal.
What is the most likely diagnosis?
1 ) Guillain Barre Syndrome
2 ) Lyme disease
3 ) Myasthenia gravis
4 ) Botulism
5 ) Vasculitis
Question 2:
A 75 year-old woman presents with a two month history of episodic loss of vision in her right eye. Her ECG was normal and carotid ultrasound reveal a 50% stenosis of the right internal carotid artery What is the most appropriate treatment for this patient?
1 ) Aspirin
2 ) Carotid endarterectomy
3 ) Dipyridamole
4 ) Prednisolone
5 ) Warfarin
Question 3:
A 70 year old woman presented with a history of pancreatitis and persistent diarrhoea. She also gave a history of osteoporosis and had had a deep vein thrombosis. Which one of the following drugs will become less effective after she starts taking Cholestyramine to relieve intolerable itching?
1 ) Aspirin
2 ) Folic Acid
3 ) Thiamine
4 ) Vitamin D
5 ) Warfarin
Question 4:
A 55 year old female presents with episodic sweats and tremors which are are relieved by glucose. She has gained approximately 6 kg in weight of late and drinks approximately 10 units of alcohol weekly. Her investigations show normal Full Blood Count, Normal Urea and electrolytes and a fasting plasma glucose concetration of 4 mmol/l (3-6). What is the most appropriate investigation for this patient?
1 ) 72 hour fast
2 ) CT scan of pancreas
3 ) EEG
4 ) Insulin and C-peptide concentration
5 ) Oral glucose tolerance test
Question 5:
A 33 year old female is admitted with erythema multiforme and erythematous lesions of the mouth and eyes.
Which one of the following drugs may account for her presentation?
1) Diazepam
2 ) Fluoxetine
3 ) Mebeverine
4 ) Oral contraceptive
5 ) Sulphasalazine
Answers to the above questions: 4,1,4,1,5. Got 100%?
Sunday, April 11, 2010
MRCP Mock Examination (1)
Hi, sorry for the long absence from this blog, these MRCP questions are the questions provided by Ahmed Hakim in his site.
Question 1:
60-year-old woman presented with 3 months history of diplopia and blurred vision of left eye. She denied any pain or other neurological symptoms. Her previous medical history is unremarkable. She smokes 20 cigarettes per day and drinks alcohol in moderation. Her general medical examination is normal. Her visual acuity on the right is 6/6 and on the left 6/36.
There is left partial ptosis and mild proptosis with conjunctival injection. The left pupil is smaller than the right but reacting normally to light. There is some limitation of abduction of the left eye. Fundoscopy showed a pale left optic disk. The left corneal reflex is reduced.
The remaining of the neurological examination is normal. Routine blood tests including FBC, U+Es, LFTs, TFTs, Ca, Creatine kinase, autoantibody screen were normal. ECG, CXR were unremarkable. Slit lamp examination was normal. Intra-ocular pressures were within normal range.
Where is the most likely cause of her symptoms?
1 ) Cavernous sinus
2 ) Superior orbital fissure
3 ) Orbital apex syndrome
4 ) Optic chiasm
5 ) Brain stem
Question 2:
A 72 year old male is being treated for hypertension, gout, Gastro-oesophageal reflux and has a three year history of type 2 diabetes. He takes a variety of medications. His general practitioner is concerned after requesting U+Es on this patient which reveal:
Serum Sodium 138 mmol/l
Serum Potassium 4.4 mmol/l
Serum Urea 12.8 mmol/l
Serum Creatinine 162 micromol/l
Of the following drugs that he takes, which one's dose does NOT need to be reduced for this patient?
1 ) Allopurinol
2 ) Gliclazide
3 ) Lansoprazole
4 ) Lisinopril
5 ) Metformin
Question 3:
A 16 year old girl is seen in clinic as she is concerned due to areas of hair loss on the scalp. Past medical history includes atopic eczema and she has a number of depigmented areas on her hands. What is the most likely diagnosis?
1 ) Alopecia areata
2 ) Hypothyroidism
3 ) Seborrhoeic dermatitis
4 ) SLE
5 ) Trichotillomania
Question 4:
A 17 year old male with glucose-6-phosphate dehydrogenase deficiency presents with tiredness and is noticed to be jaundiced. These features have developed since he developed a mild chest infection one week ago. Which one of the following is the most likely haematological finding?
1 ) Haemoglobinuria
2 ) low mean cell volume
3 ) Positive direct antiglobulin test
4 ) Reduced reticulocyte count
5 ) Spherocytes present on blood film
Question 5:
A 32 year-old man presented to hospital with a four week history of progressively worsening dyspnoea on exertion. He also complained of a non-productive cough. Over the two days preceeding admission the patient had become breathless at rest and was started on oral co-amoxiclav by his general practitioner.
On examination he was febrile 38°C and looked unwell. Candida was noted on the tonsilar pillars. No wheeze or crackles were heard in his chest. His chest radiograph is shown. Oxygen saturation was 95% on room air, but fell to 85% following about of coughing. Arterial blood gases show pO2 of 59 mmHg.
What treatment shold be given?
1 ) Co-amoxiclav + clarithromycin
2 ) Co-trimoxazole + prednisolone
3 ) Vancomycin + ceftazidime
4 ) Cefuroxime + metronidazole
5 ) Benzylpenicillin + flucloxacillin
Question 6:
A 52 year old female presents with blistering of the hands and arms which deteriorates during the summer. She was otherwise well and drinks approximately 20 units of alcohol weekly. Examination of her skin revealed erosions and scarring on the backs of her hands and forearms and some mild hirsutes.
Which one of the following is the most likely diagnosis?
1 ) Acute intermittent porphyria
2 ) Erythropoietic protoporphyria
3 ) Pemphigoid
4 ) Porphyria cutanea tarda
5 ) Subacute lupus erythematous
OK, now mark your marks, the answers to above questions are 3,3,1,1,2,4.
I will try to upload more questions soon.
Check out the latest PassPACES ebook offer!
Saturday, February 27, 2010
Multiple Myeloma in MRCP

Thursday, January 21, 2010
Rosiglitazone in MRCP

Saturday, December 19, 2009
Pass MRCP PACES in One Attempt

Sunday, December 06, 2009
Bartter's and Gitelman's Syndromes
I hate syndromes because I always can't remember them well. My Professor once said, clinicians term something as syndrome when they do not know much about an illness.
Having said that, some syndromes are important for your MRCP,I am going to talk about Bartter's and Gitelman's syndrome.
First fact to remember, Bartter's syndrome is an disorder of transport in the medullary thick ascending limb of Henle.
Second fact to remember, Bartter's syndrome is an illness resembles patients chronically takingloop diuretcs that inhibit activity of Na-K-2Cl co transporter.
Third fact to remember- they do not have hypertension.
So, what will happen to you if you chronically take frusemide?
Easy- you get hypokalemia and alkalosis and hypercalciuria- therefore leading to nephrocalcinosis. You might not be able to explain hypercalciuria but just remember that. Therefore, patients with Bartter's syndrome get hypokalemic metabolic alkalosis. ( as compared to hypokalemic metabolic acidosis in Renal tubular acidosis)

If you are interested to read more about ROMK ( renal outer medullary potassium channel), try to search the net! ( not important in your MRCP!)
As for Gitelman's syndrome, it is an disorder of distal convulated tubule, it is an variant of Bartter's syndome with similar biochemical abnormalities except Gitelman's syndrome has hypocalciuria as compared to hypercalciuria in Bartter's syndrome and hypomagnesimia in Gitelman's syndrome. ( Bartter's syndrome has normal Magnesium Level)
MRCP Past Year Question
A 15-year-old girl is referred to clinic complaining of generalised muscle weakness, fatigue and polyuria. Her blood pressure in clinic is measured at 90/74 mmHg. Investigations:
Serum sodium 127 mmol/l
Serum potassium 3.0 mmol/l
Serum urea 7.2 mmol/l
Serum creatinine 110 umol/l
Serum chloride 92 mmol/l (NR 97-108 mmol/l)
Serum bicarbonate 34 mmol/l (NR 22-28 mmol/l)
82 mmol/l (NR 0.8-1.1 mmol/l)
Urine sodium 160 mmol/l (NR 40-130 mmol/l)
Urine calcium 8.0 mmol/24hr (NR 2.5-8.0 mmol/24hr)
Which of the following is the most likely diagnosis?
Available marks are shown in brackets
1 ) Addison's disease
2 ) Bartter's syndrome
3 ) Laxative abuse
4 ) Liddle's syndrome
5 ) Thiazide diuretic abuse
What is the answer??
Friday, December 04, 2009
How to pass your Part 1 and 2?
Today I am going to talk something different. No hard facts to learn today, just relax and listen to my 5-cent advice that can help you to pass your MRCP Part 1 and 2.
First of all, I think Part 1 is more difficult to pass because candidates seldom do in basic sciences questions. I will advise you to read more about basic sciences when you sit for your part 1. Anyway, there are a few strategies to pass both your Part 1 and 2.
 1) Correct way to study
1) Correct way to studyI must say that the fatest way to remember your facts is trying to answer past years questions. When you try to do these questions, read around the topic and learn more facts about a topic. You will be suprised how fast you can master a topic.
2) Correct books to buy
Buy the correct books to study. It is difficult to tell which book to buy but remember that a good book gives your relevant and important facts to remember not high-end useless not exam-orientated facts!
3) Be systematic and disciplined
You will never pass if you are not disciplined enough, always divide your time, let say you have another 10 months before your exam, divide your time like 1 month to study endocrinology, another month to study respiratory etc. Finish all the topics before your examination!
4) Always discuss with your friends
If you do not understand a topic, always discuss with your friends who are sitting the exam together. You will be suprised how easy he/she might answer your questions. There is an old Chinese saying, when there are 3 persons together, you ceratinly can learn new things from one of them!
5) Answer all your questions
During your exam, answer all your questions, no negative marking, you have 20% chance of get it right even though you know nothing. If you randomly answer 5 questions, you will get one right!!
Hope this piece of informations helps!
Saturday, November 07, 2009
Pseudohypoparathyroidism in MRCP

Tuesday, October 13, 2009
Cryoglobulinemia in MRCP
 ( Rash on lower extremities typical of cutaneous small-vessel vasculitis due to cryoglobulinemia secondary to hepatitis C infection.- Photo from eMedicine)
( Rash on lower extremities typical of cutaneous small-vessel vasculitis due to cryoglobulinemia secondary to hepatitis C infection.- Photo from eMedicine)