MRCP Part 1 QuestionsHere are some questions for MRCP Part 1, take the test and look at the answers later!
1)Ostium secundum ASD is associated with
A tricuspid regurgitation
B left bundle branch block
C fixed splitting of the second heart sound
D onset of atrial fibrillation in the second decade
E early onset of heart failure in the second decade
2)A 34 year old male presents with episodes of breathlessness on exertion. Examination reveals a loud P2 and fixed splitting of the second sound. Which of the following may be responsible for these signs?
1 ) Maternal chicken pox infection 2 ) Maternal thalidomide therapy
3 ) 47 XXY karyotype 4 ) Homocystinuria 5 ) Excess maternal alcohol consumption
3)A 35-year-old healthy woman has a faint systolic murmur on physical examination. An echocardiogram is performed, and she is found to have a bicuspid aortic valve. In explaining the meaning of this finding to her, the most appropriate statement is that?
1 ) An aortic valve replacement is eventually likely to be required.
2 ) Other family members are likely to have the same condition
3 ) She should be treated with a cholesterol-lowering agent
4 ) The problem resulted from past injection drug usage
5 ) This is one manifestation of an underlying autoimmune disease process
4) A 24-year-old woman develops infective endocarditis involving the aortic valve. She receives a porcine bioprosthesis because of her desire to have children and not to take anticoagulantmedication. After ten years, she must have this prosthetic valve replaced. Which of the following pathologic findings in the bioprosthesis has most likely led to the need for replacement?
1 ) Calcification with stenosis
2 ) Dehiscence
3 ) Infective endocarditis
4 ) Strut failure
5 ) Thrombosis
5) The following can cause bradycardia: EXCEPT
A hypothermia B hypothyroidism C severe anaemia D subdural haematoma E shock
6)The following are recognised causes of reversible dilated cardiomyopathy:- EXCEPT
A alcohol B Selenium deficiency C Acromegaly D Lead poisoning E Coxsackie virus
7) Which of the following concerning congenital heart disease is correct?
1 ) ASD is the commonest malformation at birth
2 ) congenital complete heart block is usually associated with Anti-Ro antibodies in the mother 3 ) Ebstein's anomaly is associated with maternal exposure to lithium carbonate
4 ) Hypoplastic left heart syndrome is characterised by a large, dilated left ventricle
5 ) Osteogenesis imperfecta is associated with aortic stenosis
8) Coarctation of the aorta is: EXCEPT
A usually congenital but may be aquired
B recognised by absent or delayed femoral pulses
C a common cause of heart failure in infancy but an uncommon cause of hypertension in adults D associated with an increased incidence of an aortic bicuspid valve
E a cause of left to right shunting of blood
9)A 65-year-old woman, a heavy smoker for many years, has had worsening dyspnoea for the past 5 years, without a significant cough. A chest X-ray shows increased lung size along with flattening of the diaphragms, consistent with emphysema. Over the next several years she develops worsening peripheral oedema. BP 115/70 mmHg. Which of the following cardiac findings is most likely to be present?
1 ) Constrictive pericarditis 2 ) Left ventricular aneurysm 3 ) Mitral valve stenosis
4 ) Non-bacterial thrombotic endocarditis 5 ) Right ventricular hypertrophy
10)Increased pulmonary vascular markings on chest x-ray are a recognized feature of:
A Pulmonary stenosis
B Mitral stenosis
C Persistent ductus arteriosus
D Primary pulmonary hypertension
E chronic constrictive pericarditis
11) A 59-year-old man who was active all his life develops sudden severe anterior chest pain that radiates to his back. Within minutes, he is unconscious. He has a history of hypertension, but a recent treadmill test had revealed no evidence for cardiac disease. Which of the following is the most likely diagnosis?
1 ) Acute myocardial infarction
2 ) Group A streptococcal infection
3 ) Pulmonary embolus
4 ) Right middle cerebral artery embolus
5 ) Tear in the aortic intima
12)Low T waves on an ECG are seen in:
A hyperkalaemia B hypercalcaemia C athletes D pericardial effusion E myelodysplasia
13)A 56 year old male with left ventricular systolic dysfunction was dyspnoeic on climbing stairs but not at rest. The patient was commenced on ramipril and frusemide.
Which one of the following drugs would improve the patient's prognosis?
1 ) Amiodarone 2 ) Amlodipine 3 ) Bisoprolol 4 ) Digoxin 5 ) Nitrate therapy
14) A 70-year-old male is referred by his GP for management of recently diagnosed congestive heart failure. The patient has a history of poorly controlled hypertension. Over the last three months he has been aware of deteriorating shortness of breath, fatigue, and orthopnea. Over the last month he had been commenced on Digoxin (62.5 micrograms daily), Frusemide (80 mg daily), and amiloride 10 mg.
On examination he has a pulse of 96 bpm regular, a blood pressure of 132/88 mmHg. His JVP was not raised, he had some scattered bibasal crackles on auscultation with a displaced apex beat in the anterior axillary line, 6th intercostal space. Auscultation of the heart revealed no murmurs and he had peripheral oedema to the mid tibia.
Investigations showed: electrolytes normal serum urea concentration 17 mmol/l (NR 2-8 mmol/l) creatinine 175 micromol/l (NR 55-110) Serum digoxin 0.7 ng/mL {therapeutic: 1.0-2.0}
One month previously his urea had been 11 mmol/l and creatinine 110 micromol/l. An ECG reveals left ventricular hypertrophy and Chest X-ray shows cardiomegaly and calcified aorta.
What is the most appropriate next step in management?
1 ) Add an ACE inhibitor to the current regimen
2 ) Add atenolol at a dose of 25mg daily
3 ) Increase digoxin to 0.25 mg daily
4 ) Increase frusemide to 80 mg twice daily
5 ) Maintain on current therapy.
15)A 17-year-old woman loses consciousness while out jogging one afternoon, as she has done for many years. She is taken to Accident and Emergency, where a chest X-ray, CT brain scan, FBC, and biochemistry are all normal. Over the next year, she develops mild dyspnea and fatigue. There are several episodes of pre-syncope. After another syncopal episode, she is referred to a cardiologist who orders and ECG that shows changes of left ventricular hypertrophy and broad Q waves. An echocardiogram reveals left ventricular and septal hypertrophy, small left ventricle, and reduced septal excursion. The septum has a "ground glass" appearance. She then dies suddenly and unexpectedly. The microscopic appearance of the septum with trichrome stain reveals myofiber disarray. Which of the following conditions is she most likely to have had?
1 ) Diabetes mellitus 2 ) Hypertrophic cardiomyopathy 3 ) Rheumatic heart disease 4 ) Systemic lupus erythematosus 5 ) Viral myocarditis
16) A 78 year old female is referred by her GP with high blood pressure. Over the last three months her blood pressure is noted to be around 180/80 mmHg. She has a body mass index of 25.5kg/m2, is a non-smoker.There are no features to suggest a secondary cause for her hypertension. Which of the following is the most appropriate treatment for her blood pressure?
1 ) Alpha-Blocker 2 ) Angiotensin Converting Enzyme (ACE) Inhibitor 3 ) Angiotensin Blocker 4 ) Beta-blocker 5 ) Calcium channel blocker
17) Infective endocarditis rarely occurs with:
A mitral valve prolapse B patent ductus arteriosus C bicuspid aortic valve D atrial septal defect E mitral stenosis
18) A 60-year-old man presents with an inferior MI and receives thrombolysis. 4 hours following initial presentation he becomes acutely breathless. His ECG demonstrates sinus tachycardia (rate 108bpm) with T wave inversion inferiorly. His ST segments are normal. On examination his JVP is elevated at 5 cm. Chest was clear to auscultation. Following 80 mg of Frusemide he deteriorates. His BP is now 80/60 and his urine output over the last 2 hours is 5 mls. What is the best investigative measure?
1 ) Arterial Blood Gases 2 ) Central Venous Pressure Monitoring 3 ) Chest X-Ray 4 ) Echocardiography 5 ) Pulmonary Capillary Wedge Pressure Monitoring
19) The following are true regarding mitral stenosis:
A it is not tolerated well in pregnancy
B there is characteristically a low wedge pressure
C in AF, the opening snap disappears
D loud murmurs if valve is high calcified
E Doppler U/S is usually inaccurate in determining severity
20) The following are recognised features of pulmonary embolism: EXCEPT
A long PR interval on the electrocardiogram
B decreased left atrial pressure
C pulmonary hypertension
D collapse of the affected lung segments
E necrosis of lung tissue
Find your answers
here!

 Chronic tophaceous gout with tophi!
Chronic tophaceous gout with tophi!

 ESR-raised
ESR-raised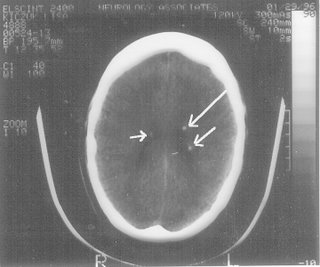
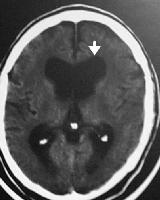

 Picture source: e-medicine (arrow- dilated ventricles)
Picture source: e-medicine (arrow- dilated ventricles)
