 Happy New Year 2008
Happy New Year 2008This blog is written for those who are preparing for MRCP Part 1 and2! Free MRCP Resource Blog!
Monday, December 31, 2007
Happy New Year!!
 Happy New Year 2008
Happy New Year 2008Tuesday, December 18, 2007
Wilson's Disease in MRCP
Actually, after practicing medicine for 6 years, I have seen only a case of Wilson’s disease. I have a patient with liver cirrhosis and after intensive investigations ( which include autoimmune screening, viral hepatitis screening, etc etc), no cause was found.
No doctor actually could find out the underlying cause of her liver cirrhosis and attributed that to cryptogenic liver cirrhosis. Later she developed tremor and was diagnosed to have Wilson’s disease after 5 years under our hospital follow up.
Anyway, I think it is a difficult disease to diagnose and I hope to discuss more about this illness today.
First thing to remember in your MRCP, Wilson’s disease is an autosomal recessive disorder involving copper metabolism. In normal subjects, ingested copper mostly will be absorbed and transported to the liver. In the liver, copper is incorporated into an alpha-2-globulin to form caeruloplasmin. Caeruloplasmin is the transport protein for copper and necessary for biliary excretion.
For patients with Wilson’s disease, there is defective intrahepatic caeruloplasmin formation. This leads to increased body and tissue copper level due to biliary excretion failure. However, urinary copper excretion is increased to compensate for defective biliary excretion.
OK, that’s the theory part of Wilson’s disease, you can think of copper as iron, when there is overload of copper in the body, it will be deposited in various organs in the body. However, remember five major organs/tissues that are frequently asked in your MRCP,
1) Brain- this can cause Parkinsonism and always remember that Wilson’s disease is one the most important differentials if you have a young patient with Parkisnonism.
2) Eye- Remember, in MRCP, they like to ask about Kayser-Fleischer rings ( although I never seen one in my life!)

3) Liver- this can lead to hepatitis, liver cirrhosis and even hepatocelular carcinoma.
4) Joints- patients can present with polyarthritis.
However, remember that you may not understand this but just remember the fact that patient with Wilson disease can have haemolysis anaemia and renal tubular acidosis and they might have pigment gallstone.
Diagnosis can only be confirmed with liver biopsy ( high copper level), however, you can detect low caerulopalsmin and high 24 hour urinary copper level.
Treatment is easy- give penicillamine or trientine for life.
Saturday, November 24, 2007
Peripheral Blood Film in MRCP(3)



 Unilateral leg swelling
Unilateral leg swellingThursday, November 01, 2007
MRCP Question Bank

Just relax, today we are going to try a few MRCP questions and I hope that you would try to answer all the questions first before looking at the answers at the end of this post.
1)
45 year old female presents with abdominal pain,depression, constipation, polyuria and thirst. Over the last 4 months she has become increasingly aware of tiredness and arthralgia since being diagnosed with hypertension and has been treated with ramipril 2.5 mg daily. Physical examination proves to be entirely normal except for a blood pressure of 162/94 mmHg. Her investigations are as follows:
Haemoglobin 14 g/dl
White cell count 7 x 109/l
Platelets 200 x 109/l
Sodium 148 mmol/l
Potassium 4 mmol/l
Chloride 105 mmol/l
Bicarbonate 28 mmol/l
Urea 8 mmol/l (NR 2-8)
Creatinine 105 umol/l (NR 50-100)
Calcium corrected 3.14 mmol/l (NR 2.2-2.6)
Parathyroid hormone 17 pmol/l (normal range 0.9-5.4)
Bilirubin 16 umol/l (NR 0-18)
ALT 10 IU/l (NR 10-40)
AST 17 IU/l (NR 10-40)
Alkaline phosphatase 130 IU/l (NR 50-100)
What is the diagnosis?
1) Depresseion
2) Primary hyperparathyroidism
3) Chronic renal failure
4) Secondary hyperparathyroidism
5) Bone metastasis due to underlying tumour
2)
A 55 year old male with a 12 year history of diabetes mellitus presents for annual review. He is currently receiving gliclazide at a dose of 80 mg twice daily. Examination reveals a pulse of 76 beats per minute regular and a blood pressure of 152/90 mmHg. Fundal examination reveals bilateral hard exudates. He has loss of vibration sensation in to the ankles but all pulses are palpable.
Investigations reveal the following:
Urine microalbumin = present
Plasma sodium138 mmol/l
Potassium3.8 mmol/l
Urea10.2 mmol/l
Creatinine160 µmol/l
Glucose12.1 mmol/l
HbA1c9.5%
Cholesterol5.5 mmol/l
Triglycerides2.8 mmol/l
Which of the following measures would you adopt to improve this patient's prognosis is?
1 ) ACE inhibitor
2 )Beta-blocker
3 )Increased dose of gliclazide
4 )Add insulin
5 )Aspirin
3)
A 22 year old female presents in the 21th week of pregnancy with profound tiredness and anxiety. Examiantion reveals a tremor, a pulse of 100 beats per minute and a soft bruit heard over the thyroid gland.
Thyroid function tests show a free T4 of 32.9 pmol/l (NR 9.8 - 23.1) and a TSH of 0.04 mu/l (NR 0.5 - 4).
Which of the following treatments would you select for this patient?
1 )Radioactive iodine therapy
2 )Carbimazole
3 )Lithium
4 )Propanolol
5 )Wait and see and repeat her thyroid function test again
4)
A 23 year old female presents with weight gain and a 4 month history of amenorrhoea. Examination reveals a BMI of 33 and mild hirsuitism. Relevant investigations reveal an oestradiol concentration of 1200 pmol/l (NR 130 - 800 pmol/l), a testosterone concentration of 2.8 nmol/l (NR less than 3 nmol/l), a prolactin concentration of 1500 mU/l (NR 50 - 450 mU/l),an LH of 1.2 u/l (NR 1.2 - 8 u/l) and a FSH of 1.5 u/l (NR 1.5 - 8 u/l).
What is the most likely diagnosis:
1) Prolactinoma
2) Polycystic ovaraian syndrome
3) Adrenal tumour
4) Pregnancy
5) Cushing syndrome
ANSWERS: 1) 2 , 2) 1 , 3) 2 , 4) 4
Tuesday, October 23, 2007
Hospital, hospital, hospital!!
Recently received an email from one of the readers of this blog asking me to write something about myself.

I also received another email from UK asking me to update this blog more frequently if possible. OK, OK......., certainly many doctors in a Malaysian public hospital will share with me the same feeling that while serving in a government hospital in Malaysia, you are mentally and physically prepared to be underpaid and overwork!
Today, there are 44 patients in my ward and three of them are critically ill. You can expect that you will never get enough ICU beds in hospital because there are simply too many patients in this country and too few beds!! I am running up and down of my ward and calling up other wards to beg for extra beds for my overflow patients.
We do not have enough beds not because we do not have enough hospitals but simply that our people just cannot afford to pay to go to private hospitals. There are more than 6 BIG private hospitals in Penang but these hospitals for the RICH only and of course, for those who have a medical card.
I do not know what the policy makers are having in their minds in this country. I anticipate that our country is going to be broke soon if we continue to practise subsidized healthcare system.
What I can see everyday in my hospital is our people are getting poorer and poorer although you may be bombared by news that our economy is great and we have produced the every first muslim astronaut in the World.
We need changes in our healthcare system. We have to make our healthcare more affordable for everyone and people can assess the healthcare system easily. No point if you say that we have the cheapest healthcare system in this World when large number of patients are clamped in a congested ward with limited numbers of staff nurses and doctors.
If we overwork and underpaid, we are providing sub-optimal care to our patients. And you can't expect our people to have first world mentality when they are getting third world salary!!
Thursday, October 04, 2007
OK, if we talk about respiratory in MRCP, there are two important topics to learn before you decide to take your MRCP part 1 and 2. I think all MRCP candidates should learn by hard flow volume loop and spirometry because you will be expecting a lot MRCP questions about these two topics.
Today, we are going to learn about flow volume loop, a flow volume loop is produced by plotting flow on the y axis against volume on the x axis.
If a subject inspires rapidly from residual volume (RV) to total lung capacity (TLC) and then exhales as hard as possible back to residual volume, then a record can be made of the maximum flow volume loop.
1) Normal Flow Volume Loop
 Normal. Inspiratory limb of loop is symmetric and convex. Expiratory limb is linear. Flow rates at the midpoint of the inspiratory and expiratory capacity are often measured. Maximal inspiratory flow at 50% of forced vital capacity (MIF 50% FVC) is greater than maximal expiratory flow at 50% FVC (MEF 50%FVC) because dynamic compression of the air-ways occurs during exhalation.
Normal. Inspiratory limb of loop is symmetric and convex. Expiratory limb is linear. Flow rates at the midpoint of the inspiratory and expiratory capacity are often measured. Maximal inspiratory flow at 50% of forced vital capacity (MIF 50% FVC) is greater than maximal expiratory flow at 50% FVC (MEF 50%FVC) because dynamic compression of the air-ways occurs during exhalation.2) Obstructive disease ( asthma, COPD)

Although all flow rates are diminished, expiratory prolongation predominates, and MEF < MIF. Peak expiratory flow is sometimes used to estimate degree of airway obstruction but is dependent on patient effort.
3) Restrictive Disease ( interstitial lung disease)
 The loop is narrowed because of diminished lung volumes, but the shape is generally the same as in nor-mal volume. Flow rates are greater than normal at comparable lung volumes because the increased elastic recoil of lungs holds the airways open.
The loop is narrowed because of diminished lung volumes, but the shape is generally the same as in nor-mal volume. Flow rates are greater than normal at comparable lung volumes because the increased elastic recoil of lungs holds the airways open.You may find the graphs very confusing, just remember a few principles here,
1) In obstructive airway disease, due to airway obstruction, the PEF ( Peak expiratory flow rate) is lower than normal ( refer to above graph).
2) In restrictive lung disease, patient total lung capacity ( TLC) is compromised due to pathology ( such as fibrosis), therefore, you notice that, TLC in restrictive lung disease is smaller as compared to normal flow loop.
( One thing to remember, the value of X axis of the flow loop get smaller toward the right!!)

Source:
1) The Merck Manual
Wednesday, September 19, 2007
MRCP Questions
Recently came across a few popular MRCP Part 2 questions. You may want to give these questions a try before looking at the answers at the end of this post.
1) A 58-year-old man with diabetes finds that the vision in one eye is blurred when he reads, but not at other times. The most likely diagnosis is:
A : Macular oedema
B : Floaters
C :Cataract
D :Glaucoma
E :Stroke.
2) A 22-year-old woman notice that her right eye vision has become blurred over the last three days and she can now see very little with it. The fundus (see image) shows:

A : papilloedema.
B : grade IV hypertensive retinopathy.
C : normal appearance.
D : optic disc swelling probably due to an acute optic neuropathy.
E : central retinal artery occlusion.
3) What does this optic fundus show?

A : Proliferative diabetic retinopathy
B : Background diabetic retinopathy
C : Grade III hypertensive retinopathy
D : Branch retinal vein occlusion
E : Central retinal vein occlusion
Answers:
1) A 2)D 3) B
Tuesday, September 11, 2007
New Drugs in MRCP- Rituximab
I am going to talk about another –ximab drug today-Rituximab. If you are currently working in a haematology unit, Rituximab is not a stranger to you because I think haematologists are the ones who use this drug most.
As Infliximab, Rituximab ( Trade name: Rituxan) is also a chimeric monoclonal antibody , it was first approved in 1997 for the treatment of lymphoma and it has become a standard treatment for aggressive lymphoma. As you might remember during your medical time that CHOP is the standard treatment for lymphoma but currently the treatment of choice it is R-CHOP! (CHOP stands for Cytoxan, Hydroxyrubicin (Adriamycin), Oncovin (Vincristine), Prednisone/Prednisolone.)
Besides lymphoma, remember that Rituximab is also useful for the treatment of Rheumatoid arthritis, autoimmune haemolysis, idiopathic thrombocytopaenia purpura, Evans syndrome and SLE ( Systemic Lupus Erythematosis). Rituximab is a unique therapy that works selectively by depleting CD20+ B cells.
The side effects of Rituximab is quite similar to Infliximab.
Check out more about this drug HERE!
Monday, September 03, 2007
New Drugs in MRCP-Infliximab
I learned pharmacology about 10 years ago. If you are one of few doctors that studied pharmacology many years ago, you might find some drugs that being asked in MRCP that you never come across before. I will talk about a few new drugs that are rather common and popular in MRCP that you might have not studied during your medical school.
The first drug is Infliximab ( Trade Name: Remicade) Infliximab is known as ‘ chimeric monoclonal antibody’ that blocks tumour necrosis factor alfa ( TNF alfa). You might come across the word ‘chimera’ in movies such as ‘Relic’ which means monster.

In Greek mythology, the Chimera is a monster, depicted as an animal with the head of a lion, the body of a she-goat, and the tail of a dragon (sometimes it has multiple heads).
In medicine, a chimera is an animal that has two or more different populations of genetically distinct cells that originated in different zygotes.
The first thing you need to know about Infliximab is its indications. Infliximab has been approved by the U.S. Food and Drug Administration for the treatment of psoriasis, pediatric Crohn's disease, ankylosing spondylitis, Crohn's disease, psoriatic arthritis, rheumatoid arthritis, and ulcerative colitis.
You must know that infiximab is classified as immunosuppressive drug, therefore always watch out for infections ( such as tuberculosis- always asked in MRCP. Always screen for possible latent TB before starting the drug!), blood disorders ( bone marrow suppression), cancers ( such as lymphoma) and allergic reaction.
Be careful if you want to start Infliximab in patients with heart failure and chronic viral hepatitis due to possibility of reactivation!
Saturday, August 18, 2007
Peripheral Blood Film in MRCP(2)
I told you a few basic terms used in haematology in my previous post. Today, I will talk about a few common and popular blood films that are commonly asked in MRCP Part 1 and 2.
1) Sickle Cell disease
 ( Blood film of sickle cell, polychromasia and target cell)
( Blood film of sickle cell, polychromasia and target cell)
By far, I think this the most popular blood film in MRCP. Remember that patients with sickle cell may present with bone pain ( due to bone necrosis), osteomyelitis, leg ulcers or even iron overload. Remember that it is one of the important causes of chronic haemolysis anaemia, therefore, you might find pallor with jaundice in patients with Sickle Cell Disease. However, remember that you may not find splenomegaly ( although you anticipate splenomegaly in patients with chronic haemolysis) because there is a possibility of splenic infarct!!
 ( Patient presents with painful bony infarction)
( Patient presents with painful bony infarction)2) Thalassemia
This disease needs no further explanation. I have seen so many Thalassemic patients during my paediatric posting when I was a medical student.
Look at the following blood film,
 ( Blood film showing hypochromic, microcyctic red cells)
( Blood film showing hypochromic, microcyctic red cells)You may be given a photo of patient with classical thalassemic facies and you are expected to know about types of Thalassemia, chromosome involved and complications!
3) Malaria
OK, if you are living in UK or Ireland, you may not seen a case of malaria in your whole life. However, malaria is endemic in tropical countries including Malaysia and Thailand. You may still remember that there are various species of Plasmodium such as P.falciparum, P.vivax and P.ovale. Anyway, remember that in your MRCP, they always show you the ring form!

Tuesday, August 07, 2007
Infectious Disease in MRCP- Leptospirosis
OK, I told you before a few common infections which are popular in MRCP examination. These infections include HIV, Tuberculosis, Infective endocarditis. Today, we are going to discuss another common infection which is popular if you are sitting MRCP Part 1 and 2 examination.
Yes, Leptospirosis is important because it is the most wide spread zoonosis caused by Gram-negative organism Leptospira interrogans. It is harboured by wide varities of animals but mainly by rats. Therefore, anyone exposed and has contact with animals, animal products ( like rats’ urine) or soil/water contaminated with leptospiras may get the infection.

Recreational activities like swimming, rafting, canoeing in contaminated rivers/lakes may expose someone to leptospiras.
Signs and symptoms of Leptospirosis
Always remember that patients always go through biphasic course during the illness. Phase 1 ( about 1 week) is considered as febrile/septicaemic phase where patients experience with high fever and non specific symptoms such as myalgia, headache, diarrhoea, arthralgia. ( symptoms that are common in viral infections)
During the second phase (4- 30 days), patients go through what is considered as immune phase where they may have aseptic meningitis, acute renal failure,pulmonary haemorrhage, myocarditis, liver failure ( therefore you may find jaundice) and ARDS.
Investigations
Always check FBC, LFT ( ALT usually mildly elevated), CK which may be raised due to carditis or muscle break down.
Remember that Leptospira can be cultured from blood or CSF during the first week of illness and from urine from 2-4 weeks of illness ( popular question in MRCP). However, diagnosis is usually confirmed by serology.
Complications
Acute renal failure ( common during immune phase), ARDS, DIVC
Treatment
IV penicillin or ceftrixaone or doxycyline for mild disease.
Wednesday, July 25, 2007
Pulmonary Embolism in MRCP
I saw a case of suspected Pulmonary Embolism today, therefore, we will talk about PE today in our MRCP blog today.
I think that Pulmonary Embolism is important not just because you are sitting for MRCP Part 1 and 2 but also as a clinician in everyday practise because it is often missed and not treated.
As defined in Wikipedia, Pulmonary embolism (PE) is blockage of the pulmonary artery (or one of its branches) by a blood clot, fat, air, amniotic fluid, injected talc or clumped tumor cells. By far the most common form of pulmonary embolism is a thromboembolism, which occurs when a blood clot, generally a venous thrombus, becomes dislodged from its site of formation and embolizes to the arterial blood supply of one of the lungs.

However, when we talk about venous thromboembolism, always remember that there are three aspects you must always remember when blood clots inside a vessel. It can be due to either alterations in blood flow, factors in the vessel wall and factors affecting the properties of the blood--- these three factors are well known as Virchow's triad.
Remember that PE usually occurs due to embolism from a blood clot from the lower limb and predisposing factors for deep vein thrombosis is the most popular questions asked in MRCP.
It is easy to remember that there are two major risk factors predispose you to have thrombosis, either inherited or acquired, always suspect inherited causes if young patients present with thromboembolic events and there is presence of family history. Just remember that some inherited causes like Protein C,S, anti-thrombin deficiency and Factor-V Leiden mutation.
But put more emphasis on acquired causes because they are the more important and commoner causes for thromboembolic events, remember the mnemonics below,
EMBOLISM
E- Extra causes- inherited causes
M-Malignancy
B- Baby ( Pregnancy)
O- Oral Contraceptive pill
L- Large- obesity ( maybe lead you to immbolity)
I- Immune disease-Antiphospholipid
S-Surgery
M- Mobility ( immobilization)
Patients with PE usually present with SOB, haemoptysis, chest pain and even sudden death.
There are various investigations can be done to diagnose PE, however, remember you may find Westermark sign ( localised pulmonary oligaemia) in CXR and classical ECG finding ( S1QIIITIII) . Although you seldom see these in clinical practice, I do not understand why these questions are alwyas asked in your MRCP.
However, in 1995 Wells et al suggested a scoring system to diagnose PE and if you are sitting for MRCP PACES, learn this criteria hard!!
The treatment is easy, use heparin and give them warfarin for at least 6 months.
Saturday, July 14, 2007
ECG in MRCP(3)
I have covered common MRCP questions about ECG in my previous 2 posts, today, we are going to talk about heart block, there are two main type of heart block, AV ( atrio-ventricular) block and intraventricular block. We will talk about AV block today. As you might remember as a medical student, there are three subtypes of AV block, namely first, second and third degree heart block.
First degree heart block
It is easy to pick up in your ECG, normal PR interval is 0.12-0.20s, if PR interval is more than 0.2s, it is considered as first degree heart block.
 Note: Always remember that shortened PR interval occurs in WPW syndrome!
Note: Always remember that shortened PR interval occurs in WPW syndrome!Second degree heart block
There are two types of second degree heart block,
a) Classical “Wenckebach” ( Mobitz type 1) where the PR interval gets longer (by shorter increments) until a nonconducted P wave occurs. The RR interval of the pause is less than the two preceding RR intervals, and the RR interval after the pause is greater than the RR interval before the pause.
 b) Mobitz type 2- For this heart block, AV block the PR intervals are constant until a nonconducted P wave occurs. ( as below ECG)
b) Mobitz type 2- For this heart block, AV block the PR intervals are constant until a nonconducted P wave occurs. ( as below ECG) Third degree heart block
Third degree heart blockEasy to remember, complete AV dissociation

Friday, May 25, 2007
Blood Film in MRCP(1)
Certainly before your MRCP Part 1 and 2, you need to know a very important topic in haematology, you are right, many candidates have the tendency to go to the examination without knowing anything about blood film.
You must know a few popular blood films in MRCP, before we proceed to revise a few important blood films, I think you must remember these useful terms here,
1) AniSocytosis- Variation in Size.
2) Poikilocytes- Variation in shaPe
3)
 Basophilic stippling of RBCs is seen in lead poisoining, thalassemia and other dyserythropoetic anaemias
Basophilic stippling of RBCs is seen in lead poisoining, thalassemia and other dyserythropoetic anaemias4) Blasts- Nucleated precursors cells
5) Howell Jolly bodies- Nuclear remnants seen in in RBCs especially in post splenectomy
6) Leukaemoid reaction- A marked reactive leucocytosis
7) Left shift- Immature white cells seen in circulating blood
8) Right shift- Hypersegmented polymorphs ( Image below)

9) Rouleaux formation- Red cells stack on each other
10) Target cells RBCs with central staining, a ring of pallor and an outer rim
Thursday, May 03, 2007
Spondyloarthropathies in MRCP (2)
1) Reiter’s syndrome
Remember the triad of conjunctivitis, urethritis and arthritis. This was described by Hans Reiter in 1916.
Reactive arthritis is triggered following enteric or urogenital infections. Reactive arthritis is associated with human leukocyte antigen (HLA)–B27, although HLA-B27 is not always present in an affected individual.
Bacteria associated with reactive arthritis are generally enteric or venereal and include the following:, Salmonella typhimurium, Salmonella enteritidis, Streptococcus viridans, Mycoplasma pneumonia, Cyclospora, Chlamydia trachomatis, Yersinia enterocolitica, and Yersinia pseudotuberculosis.
Remember that always suspect this in young patients who come in with large mono- or oligoarthritis especially knee pain.
Other features of this syndrome include Keratoderma blenorrhagica


Asymmetric, oligoarticular, and more common in the lower extremities pattern of joint involvement
Juxta-articular osteoporosis in acute episodes of arthritis - Erosions have indistinct margins and are surrounded by periosteal new bone.
Spinal pattern - Unilateral or bilateral sacroiliitis, asymmetric paravertebral comma-shaped ossification involving the lower thoracic and upper lumbar vertebrae
Treatment: bed rest and NSAID
2) Psoriatic arthropathy
Kindly visit PassPACES.com for further discussion
3) Enteropathic spondylitis
Saturday, April 07, 2007
Basic Anatomy in MRCP(II)
I have covered the first six cranial nerves in my previous post, today we are going to talk about another a few interesting points about the first six cranial nerves that are frequently asked in MRCP.
1) Correlation of third cranial nerve with pupil size is an important topic to study. Generally, if you can still remember as a medical student, isolated third nerve palsy is always divided into either a 'medical' or 'surgical' third nerve palsy. As you can remember from my previous post, I told you that third nerve palsy should cause patient to have dilated pupil due to its parasympathetic component.

A COMPLETE third nerve plasy ( Above patient - right third nerve palsy) should have:
i) Dilated pupil (mydriasis)
ii) Ptosis
iii) Deviation of eye laterally and downward ( due to unopposed actions of lateral rectus and superior oblique)
2) Isolated 6th nerve palsy is possible and commonly found in patient with increased intracranial pressure. It is termed as ' False localizing sign' because actually you can’t localize any location at the brain that causing this palsy if you observe only isolated 6th nerve palsy. It occurs only to 6th cranial nerve in increased intra cranial pressure because of its long course intracranially and makes it prone to compression when there is an increased pressure inside the skull.
Sunday, March 11, 2007
Arterial Blood Gas in MRCP (2)
In my last post, I talked about Metabolic Acidosis and respiratory acidosis. Today I will cover metabolic alkalosis and respiratory alkalosis.
Take it easy because these two conditions are rare in your MRCP examination.
1) Metabolic alkalosis
The only one time you will be see metabolic alkalosis in your clinical practice is after patient has severe prolonged vomiting (especially in pyloric stenosis). This is because our gastric juice is acidic, where there is excessive loss of acid from our stomach, we turn alkalosis. You notice PH↓ and HCO3↑. You body may compensate by keeping more CO2 therefore there is a possibility that in your ABG, PaCO2↑

2) Respiratory Alkalosis
This is commonly seen in your clinical practice especially in A+E department but it is not an emergency. You usually see young ladies come to A+E complaining of shortness of breath but it is actually due to hyperventilation ( may be due to anxiety or not). However, never always assume that young ladies have hyperventilation when they complain to you that they are breathless. My old professor always told me that because some young ladies may also have pulmonary embolism ( due to risk factor of taking oral contraceptive pill or underlying autoimmune disease) when they are breathless. Therefore, always do an ABG if you are in doubt.
MRCP candidates always worried because in MRCP Part 1 and 2 examinations, they may show combination of abnormalities. There is always one rule to remember, if you can’t explain the abnormalities, always suspect this possibility.
Let me illustrate to you a case, let say a diabetic patient is admitted to you’re A+E due to cough and fever for 1 week and his CXR shows pneumonia. His ABG result is as below,
PH=7.2
HCO3=10
Random blood sugar = high
PaCO2=7 kpa
PaO2= 8kpa
Ok, from these first three results, we notice that this patient has metabolic acidosis ( PH↓, HCO3↓) and it is most probably due to diabetic ketoacidosis because the sugar is high as well. However, you will anticipate the PaCo2 to be low ( due to air hunger) but in this case the PaCO2 is high as well, you can’t explain that ( this is not a normal physiological respond) but from logical thinking, you know that this is a combination of metabolic and respiratory acidosis! ( Patient’s lung is also failing due to severe pneumonia and it is unable to compensate for the metabolic acidosis!)
Thursday, February 22, 2007
Arterial Blood Gas in MRCP(I)
Recently I received an email from a MRCP Part 1 and 2 blog reader about ABG interpretation in MRCP. I share with him the same feeling that ABG interpretation is important in MRCP as well as your daily clinical practice.
Our blood PH is closely regulated in a tight range around 7.4±0.05 so that our body can function properly. As you might remember during your secondary school time, enzymes function in certain PH range and will be damaged by acidic or alkaline environments.
Although a lot of candidates ( and a lot of house officers) tend to make various mistakes in ABG interpretation. I would like to give a few simple rules to remember so that you will not make any more mistakes in future,
1) There are two important organs in our body which control our body PH- lung and kidney.
2) Carbon dioxide is an acidic gas, therefore, in acidic environment ( due to various insults), our body ( the lung) tends to compensate by exhaling out more CO2 ( therefore, patient tends to hyperventilate) and vice versa.
3) HCO3 is alkaline and its level is mainly regulated in our kidney.
4) PH=7.4 is normal, if PH less than 7.35 is acidic and more than 7.45 is alkaline.
5) Remember other normal values, normal HCO3=22-28 mmol, PaO2 more than 10.6 kpa ( 1kPa=7.6mmHg), PaCO2=4.7-6.0 kPa ( 35-45mmHg)
OK, for you to interpret ABG results correctly, follow these simple steps,
1) Read the PH first, if PH<7.35, it is acidosis, if it is more than 7.45, it is alkalosis.
2) Once you know whether it is acidosis or alkalosis, you must determine eithet it is respiratory or metabolic, I find two useful parameters to look at, HCO3 and PaCO2.
Let me show you a few examples,
1) Metabolic Acidosis
I still think this is the commonest and most important acid-base balance disorder you will find in your MRCP and daily clinical practice. Read the causes for metabolic acidosis in my previous post.
However, in daily practice, you commonly find metabolic acidosis in uraemia ( chronic kidney disease patient) , diabetic ketoacidosis, salicylates poisoning and lactic acidosis.
Therefore, in metabolic acidosis, you will find PH↓, HCO3↓ and PaCO2↓, it is easy to understand, in metabolic acidosis, our body cannot conserve HCO3, therefore the level of HCO3 is low, however, for our body to compensate ( try to push up PH level), we will hyperventilate to blow out more CO2 ( because CO2 is acidic), therefore, patient will hyperventilate in metabolic acidosis. (air hunger)
You must remember that there are two types of metabolic acidosis- reduced anion gap and normal anion gap ( normal anion gap=8-16 mmol) metabolic acidosis, I have covered this topic in my previous post.
MRCP Question
A 16-year old girl is admitted to your ward from A+E department due to vomiting and abdominal pain. She has no known medical problems and denies taking any illegal drugs.
On examination, you noticed she is dehydrated, blood pressure=90/50, pulse rate=120 and her abdomen is soft. Below are her blood results,
Full blood count
Total white 16,000 ( Normal 4000-11,000)
Hb=12.3
Plt= 235,000
K= 3.2
Creatinine= 110
Na= 131
Cl=100
ABG ( on room air)
PH=7.21
HCO3= 12
PaO2= 12.2 kPa
PaCO2=2.5 kPa
Q: What is the diagnosis?
For the above ABG result, you know that the patient has metabolic acidosis and she presents with history of vomiting and abdominal pain, the first provisional diagnosis you should think of as a SHO is diabetic ketoacidosis!
2) Respiratory Acidosis
This is the second commonest acid-base balance problem you will see in your daily practice. Patients develop this because he/she is unable to blow out CO2 in the lung leading to accumulation of CO2 and respiratory acidosis. Therefore, our body will try to compensate by keeping more HCO3 via the kidney to buffer the acidosis. However, you must remember that kidney works somehow slower than the lung, therefore in acute respiratory acidosis (acute CO2 retention), you may find the HCO3 level is normal but in chronic CO2 retention ( such as in CAPD/COAD or chronic lung disease patients), the HCO3 level tends to be high.
This remembers me when I was a medical student where my lecturer liked to ask me way to help clinicians to differentiate COAD/COPD from asthma by looking at ABG results.
If you are a SHO on call in chest ward, a patient comes in with acute breathlessness and you notice he/she has rhonci all over the lung, you will most probably find the following ABG if you put patient on oxygen supplement,
PH ↓, PaO2 ↑, PaCO2↑ ( Respiratory acidosis)
For COAD /COPD, since that patients may have chronic CO2 retention, you will notice the HCO3 level tends to be high but in asthmatic patients, since it is an acute asthmatic attack that leads patient to have acute CO2 retention, you may find the HCO3 level to be normal ( kidney needs sometime to conserve HCO3, therefore in acute CO2 retention, the HCO3 level may be normal)
However, I must warn you that this rule is only for your reference only, there is no 100% in clinical medicine but I find this rule rather useful in daily practice.
I will talk about metabolic and respiratory alkalosis in my next post!
Sunday, February 18, 2007
Happy Chinese New Year!

For all MRCP Part 1 and 2 blog readers, Happy Chinese New Year! May your wish comes true this year!
Tuesday, February 13, 2007
Addison's Disease in MRCP
OK, today I am going to talk about one condition which is important in two ways, Addison’s disease is an important endocrine condition because,
1) It is a popular condition in your MRCP examination,
2) It is important clinically because the mortality is high if you do not pick it up fast in clinical practice especially if patients present with acute Addison's crisis!
Adrenal insufficiency can be due to dysfunction of the adrenal gland itself ( primary- Addison’s Disease) or due to disordered pituitary or hypothalamus function ( secondary)
I think we will cover Addison’s disease today and you can forget about secondary Adrenal insufficiency because it is rather rare.
Addison’s disease refers to primary failure of the adrenal gland leading to loss of production of glucocorticoids and mineralcorticoids.
Causes of Addison’s disease
1) Always remember that it is mainly due to autoimmune adrenalitis and it is associated with Polyglandular autoimmune syndrome. ( Never get yourself confused this with Multiple Endocrine Neoplasia, MEN)
Remember as well that you may find antibodies against the 21-hydroxylase enzyme in 90% of autoimmune cases.

2) Tuberculosis
3) Distant metastasis
Signs and symptoms
As I remember as a medical student, there are 3 main medical causes( non-surgical causes) of abdominal pain, of course Addison’s disease is one of them. The other two are Diabetic ketoacidosis and intermittent Porphyria. ( Always remember this and later you will realize that it is very common for your friends in A+E missing diabetic ketoacidosis simply because patients present with abdominal pain)
Other symptoms include lethargy, nausea and vomiting, dizziness.
Important signs to look for are
1) hyperpigmentation ( it is a popular case in MRCP PACES as well) and I hope you know the reason behind this.
2) postural hypotension
3) loss of body hair ( due to reduced production of androgen)
Investigations
Remember the important clues to look for are
1) Low Sugar
2) Low Sodium
3) High Potassium
------- SSP. Patient may present with fever as well.
Diagnosis
Synacthen test. I think you do not need to know the details and the values. Just know the principles, in normal people, cortisol level will increase significantly after synacthen ( ACTH) stimulation but for Addison’s disease, since there is primary failure of adrenal gland, it will not be stimulated to produce more cortisol after synacthen.
Management
Remember that acute Addsison’s crisis is a medical emergency and it is usually due to prolonged adrenal suppression secondary to exogenous drugs such as steroids.
For chronic Addison’s disease, supplement patients with glucocorticoid ( hydrocortisone) and mineralcorticoid ( fludrocortisone)
Tips for MRCP
You may give a case in your MRCP Part 2 where you are given some electrolytes imbalances in a patient who presents to A+E due to abdominal pain.
Thursday, February 01, 2007
ECG in MRCP(2)
In sinus rhythm, we know that every P wave is followed by QRS, you must learn hard the following conditions that do not give you sinus rhythm,
1) Atrial fibrillation
This is the commonest condition being asked in MRCP, I have covered this in my previous post.
2) Atrial flutter
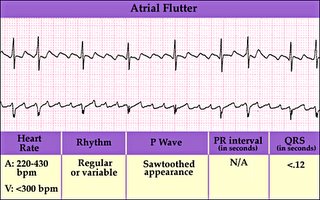
Always described as “ Saw-Tooth” ECG in medical textbook. The atrial activity is usually between 250-350 beats /min and there is sually 2:1 or 3:1 block. Causes for atrial flutter are similar to atrial fibrillation as well as the management.
3) Ventricular tachycardia

Defined as three or more successive ventricular extrasystoles at a rate more than 120/min. Remember than VT has a wide QRS complex. Causes of VT include
a) Ischaemia to the heart
b) Hypo-or hyperkl\alaemia
c) Long QT interval ( a very popular question in MRCP, I will cover this in depth in my future post)
d) Cardiomyopathies
4) Torsades des pointes
Actually it is a type of ventricular tachycardia with a varying axis. It often happens after heart attack but can be due to drugs and other causes of prolonged QT interval.
5) Ventricular fibrillation
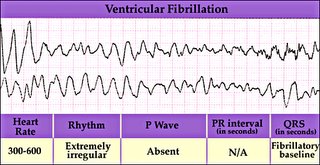
This rhythm needs immediate cardioversion. Usually happens after a hear attack
Important Tips for MRCP,
It is often difficult to differentiate an SVT with abberant ventricular conduction from VT ( both also have wide QRS complexes), however always remember in clinical practice, always assume VT if you are in doubt and treat accordingly because VT is commoner and life threatening. However, following features suggest SVT with abberant blocks,
1) No fusion or capture beats
2) Presence of P waves associated with ORS
3) Classical RBBB and LBBB ORS morphology
4) ORS <0.14s
5) Same QRS morphology as in sinus rhythm
6) Normal axis
Tuesday, January 23, 2007
Basic Anatomy in MRCP (I)
Anatomy was a hell for me when I was a medical student. There is no trick to be good in anatomy except you have a good memory. Luckily, there are not so many questions about anatomy being asked in MRCP Part 1. I will try to cover basic anatomy in a few posts and I hope the information provided in this blog will be useful for you to answer your MRCP questions.
OK, today I will try to cover the first 6 cranial nerves today and I will try to give you a few popular questions in MRCP.
Refresh your memory first and remember all 12 cranial nerves ,

Nerve I, Olfactory nerve- just remember that it is for smell
Nerve II ( Optic) and Nerve III ( Occulomotor) are important nerves to remember,
There are a few common questions asked in MRCP about these two nerves,
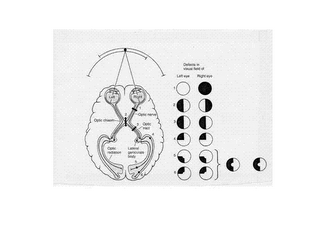
a) Remember that Optic nerve is for vision and you must always remember the visual fields , it is important in your MRCP Part1,2 as well as in MRCP PACES
b) Remember your afferent fiber for your pupillary reflex is your optic nerve and your efferent fiber is Occulomotor ( therefore occulomotor nerve is a parasympathetic fiber)
c) Remember that other components of Occulomotor nerve ( besides its parasympathetic function in constricting pupil) are motor components supplying all extraocular muscles except lateral rectus and superior oblique. It also supplies levator palpebrae superoris.
Therefore, a complete third nerve palsy gives,
i) Dilated pupil (mydriasis)
ii) Ptosis
iii) Deviation of eye laterally and downward ( due to unopposed actions of lateral rectus and superior oblique)
SO…….., one very,very important formula to remember in eye movement is (LR6SO4)3, lateral rectus is supplied by sixth nerve (abducent nerve) and superior oblique is supplied by fourth nerve (Trochlear nerve) and others are supplied by third nerve ( Occulomotor)
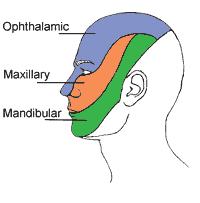
You will be surprised that we have learned 5 nerves out of first six cranial nerves, the fifth cranial nerve is trigeminal nerve, just remember that its sensory component supplying the facial sensory dermatomes ( One popular question in MRCP is they will show a patient with shingles over the face and you are expected to know what sensory component of trigeminal nerve is involved!)
Friday, January 19, 2007
New MRCP Sites
For those who are preparing for MRCP Part 1 and 2, I want to recommend you to visit the following sites which are written by Dr Osama Amin. Although I do not know him personally, I think he has done an excellent job to provide FREE information for those who are sitting for MRCP exams. I think he has similar intention as me----hoping that all of you can pass your MRCP if you really study hard!
1) Neurology for MRCP Mocks
2) Neurology for MRCP Blog
Good luck!
Monday, January 08, 2007
Infective Endocarditis in MRCP
Today I would like to discuss about infective endocarditis which is defined as infection of the endothelial surface of the heart. It is a common condition asked in MRCP!A heart valve is always involved but the infection may develop on a septal defect or on the mural endocardium.
Generally, it is useful to classify endocarditis into these three subtypes,
1) Native valve endocarditis- endocarditis develops in native valves. Patients developing native valve endocarditis usually have valvular heart lesion. Common valvular heart lesions that prone patient to get endocarditis include mitral valve lesions ( incompetence and stenosis), aortic valve lesions ( incompetence and stenosis)
2) Endocarditis in Intravenous Drug Abusers- usually IVDUs develop right heart endocarditis ( Tricuspid Valve) due to direct septic emboli to the right heart from peripheral vein.
3) Prosthetic Valve Endocarditis- Endocarditis develops in prosthetic valves. It is easier for you to remember the causative organisms if you divide Prosthetic valve endocarditis into early or late. For early onset Prosthetic valve endocarditis ( onset of symptoms within 2 months post valve replacement), the causative agent is mainly S.epidermidis. Late onset Prosthetic valve endocarditis usually happens post instrumentation in patients with prosthetic valve.
Signs and Symptoms of Infective Endocarditis
Patients may present with fever, lethargy ( may be due to anemia), unexplained weight loss, chest pain, confusion
Always remember about stigmata of infective endocarditis- Janeway lesion ( non- tender), Osler’s nodes (tender), splinter haemorrhages, Roth Spots and petechiae( due to septic emboli)
Splenomegaly
Murmurs
Clubbing
Fever
 (A-splinter haemorrhage, B-Conjunctival petechiae, C-Osler's node, D-Janeway's Lesion)
(A-splinter haemorrhage, B-Conjunctival petechiae, C-Osler's node, D-Janeway's Lesion)
( There is a criteria for you to diagnose Infective Endocarditis known as Durack’s criteria, you do not need to know about the details, however, remember that the two major criteria are positive isolation of organisms from blood culture and evidence of endocardial involvement on ECHO)
Investigations
Full blood count- raised TWC and anemia ( normocystic, normochromic), raised ESR
Haematuria may be present in 50% of cases
Blood culture ( remember that you may need CO2 culture for fastidious HACEK organisms-Haemophilus, Actinobacillus,Cardiobacterium,Eikenella and Kingella)
Complications
Mainly due to septic emboli- the emboli can go to brain, spleen, liver, lung leading to abscess formation. In the heart, infective endocarditis can cause valvular failure, heart block and prosthesis failure!
Treatment
Prolonged IV antibiotics ( up to 4-6 weeks) , usually combination of IV penicillin + gentamycin.
Surgery is indicated if development of fungal endocarditis, valve dehiscence, heart block, valve ring abscesses, failure of medical treatment!
Tips for MRCP
1) Remember patients with what valvular heart lesions need antibiotics prophylaxis before invasive procedures. Click here to find out more!
2) Remember what do you mean by invasive procedures, click here to learn more!
Monday, January 01, 2007
Happy New Year 2007!
Hi, Happy New Year to all and for those who are sitting MRCP soon, good luck! I would like to wish all of you " Happy New Year" and hope that 2007 will be a wonderful year for everyone. I started MRCP Part 1 and 2 blog 6 months ago and I really like to thank all of you for reading this blog.

Anyway, while sufing the internet,besides learning about medical knowledge, I hope that all of you can get some benefits out of it. I want to introduce to you about AGLOCO. Do you realise how valuable we are?Advertisers, search providers, and online retailers are paying billions to reach you while you surf. Howmuch of that money are you getting? Zilt, so far that is........ZERO!
Therefore, as a MRCP Part 1 and 2 blog reader, I hope we all can build up a community and get some money while surfing the internet!
Here is why I would like you to consider joining:
1. AGLOCO pays you, as an Internet user, your fair share of the value created while you surf.
2. The AGLOCO's free software puts you in control of what arrives on your screen and what data you allow outsiders to collect.
3. AGLOCO is a 100% Member owned company which rewards the Members who help build the company. It never costs anything to be a Member AGLOCO is only four weeks old and it has already signed up tens of thousands of Members and has created enormous Internet 'buzz' (over 700,000 pages in Google's search talk about AGLOCO).

AGLOCO is not a 'get rich' quick scheme. Every additional Member raises the value of all the Members, so we all get more if you join.
Learn more abouth this program at http://www.investing-tip.com/makemoney.html
It is free to join and Membership never costs anything. Click here to read more and sign up now. CLICK HERE NOW TO JOIN!
Thanks
PassMRCP
